MIS Surgical Treatment for Kyphoscoliosis in a patient with Parkinsons Disease
24/3/2019
MIS Surgical Treatment for Kyphoscoliosis in a patient with Parkinson's Disease
The most common neurodegenerative disease is Parkinson's disease (PD). Its clinical manifestations are tremor, rigidity, and akinesia. Patients with PD could have stooped posture and different types of postural and striatal deformities may also be developed. Multiple studies show that these may also be apparent in roughly a third of PD patients resulting in severe disability.
These can include antecollis or dropped head, Pisa syndrome, camptocormia, kyphosis or/and scoliosis, striatal hands, and striatal toes.
The pathogenesis of these deformities is a combination of central and peripheral impacts such as rigidity, dystonia, and degenerative skeletal changes.
The standard practice in these patients to aim at a long-lasting effect is an open instrumented fusion of the spine usually combined with osteotomies and/or anterior fusion to decompress neural elements, maintain or restore the patient’s balance.
In combination with the comorbidities seen within this age group, these operations are related to a high rate of complications.
A blood loss of more than 2 liters is considered to be one of the risk factors.
Duration of parkinsonism symptoms is a major risk factor and these deformities are seen in an advanced stage of the disease in most patients.
Patients who present these symptoms may respond to dopaminergic medications at first. However, they may become fixed and hard to treat if there is no quick intervention.
The most common clinical manifestations are pain and restriction of movement, similar to symptoms of musculoskeletal disorders like rheumatoid arthritis. Early diagnosis is of great importance since the patients may respond to adjustment in dopaminergic medications.
During the last decade, MIS techniques have gained space in the treatment of Deformities in order to decrease perioperative complications associated with conventional techniques.
MIS approach has not been reported in Kyphoscoliosis in patients with Parkinson’s Disease. This is possibly due to concerns with longer surgery time, which is further increased due to more levels fused and instrumented, challenges of pelvic fixation, size and number of incisions, and prolonged anesthesia.
Patient female 75 years old with a history of Parkinson’s Disease treated with medication for 10 years.
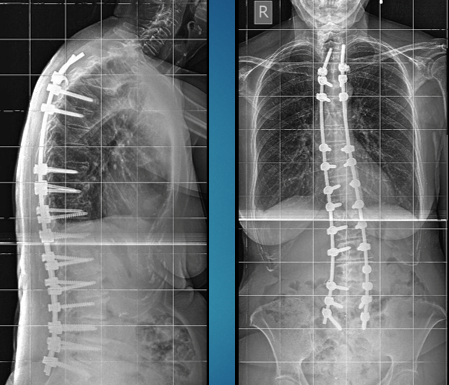
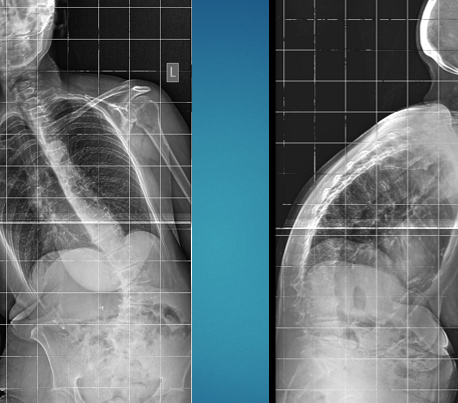
During the last one and half year, she started to have a change in her posture and she progressed to severe kyphoscoliosis (Cobb Angle 41,8 and 71,2)
Technique
Percutaneous Screws T5-S1,
Percutaneous Hooks T5
Discectomy L5-S1 and TLIF L5-S1
In situ bending in the upper thoracic spine, typical maneuvers for correcting the deformity
Results
Neuromonitoring was used with no changes during the surgery.
The total duration was 7 hours and the estimated blood loss was 300 mL.
The patient received 1 unit of packed red blood cells intraoperatively and was successfully extubated at the end of the procedure.
PICU stay was one day and ambulate on POD #2.
The hospital stay was 4 days.
A minimally invasive approach seems to provide the greatest benefits to PD patients with Kyphoscoliosis in terms of blood loss, pain, ICU, and hospital stay.